The normalcy to the world after challenging days of pandemic would be a coexistence with COVID-19 as the virus remains a venomous threat unless there is a vaccine. The unpredicted dystopia has portrayed the vulnerable global healthcare system inside out where thousands of hundreds of people’s lives are wiped out especially those of baby boomers in a matter of weeks. One U.S news article report wrote “the current Coronavirus is suddenly and permanently changing the way we deliver, the way we consume and we pay for healthcare services in the United States. The pandemic has also opened doors to innovation…”. Obviously, the healthcare system is scaled up to limit the transmissions and to meet shifts in demand for treatment due to travel restrictions and lockdown measures. Indeed, some things will never be the way they once were.
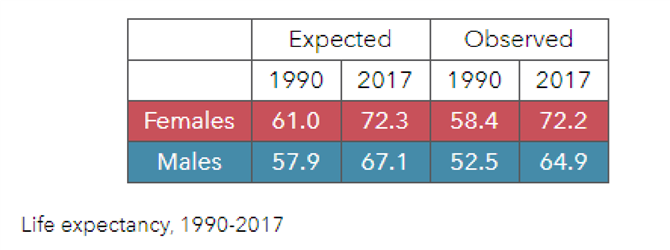
Speaking of vulnerability to Covid-19, Myanmar seemed to get less affected in a way of cluster transmission from the first wave when compared to many parts of the world. Myanmar managed to survive at the lowest death toll in the region by suppression stringency means which are within reach in the face of global pandemic as a country struggling with poverty with approximately 25% of its population living below the poverty line with a prominent rural-urban divide. Although nominal GDP percentages are trending upwards in the years before Covid-19 interruption, Myanmar ranks one of the lowest in the region when it comes to health as evident in government spending, bed capacity, human resources, technologies such as diagnosis and disease monitoring.
The healthcare system in Myanmar has been making its headway since the 1990s. Success stories were along the way, however, there was still a significantly lower spending on healthcare in 2013 when compared to the data of other countries such as Laos (4.5% of GDP) and Cambodia (5.6% of GDP) accounting for only 3.05% of GDP. It is undeniable that the sector has gained attention from the authorities by looking at rising healthcare expenditure and coordination of three national healthcare plans NHPs. As of today, according to the Healthcare guide 2020 by EuroCham, the total healthcare expenditure of Myanmar in 2017 was $3.3 billion or $63 per capita which is higher than Indonesia, but much lower than some of the other ASEAN countries. The amount of government expenditure is still relatively limited spending over $20 per capita in comparison with its ASEAN neighbours. Like in other regional states, the private healthcare market in Myanmar has mushroomed with an expenditure of $3.1 billion in 2018, observed to be rising from $2.5 billion in 2015 whereas government expenditure was at approximately $741 million which is 6% of the total government budget, representing 1% of the GDP in 2017.
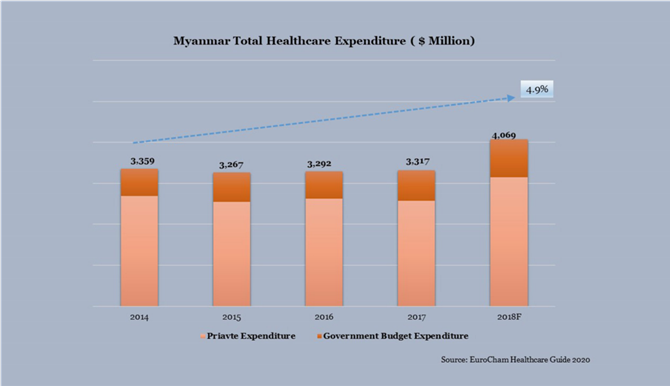
The main source of financing healthcare services roots in household out-of-pocket (OOP) payment which can be naturally found in low-income countries. Actually, healthcare expenditure constituted 9% of the typical Myanmar consumers’ monthly household expenses in 2014, the second largest category of consumer spending, after food & groceries, according to Nielsen. In Myanmar, OOP accounts for 78% of the total healthcare expenditure. Simply put, for every $10 spent on health, people have to pay more than $7 while the rest by the government. OOP expenses are used for self-prescribed medicine, diagnostics and private clinics.
When it comes to infrastructure, the health facilities comprise a mix of public and private for-profit and nonprofit domains, along with booming outbound medical tourism, in financing and provision. According to data available from the Ministry of Health and Sports, the overwhelming majority of hospitals are public, accounting for over 1,100 hospitals registered nationwide. Shan State ranks the highest share at 14%, followed by Sagaing Region at 12% and Ayeyarwady Region at 11% of the public hospitals in Myanmar. Although the existing public hospitals host over 55,000 beds as of late 2019 data, the supply is insufficient. The bed capacity is around 0.9 beds per 1000 of the population. Moreover, there is provision of 0.6 doctors and 0.9 nurses per 1000 of the population, according to the Oxford Group Report 2020. These metrics pose a considerable burden on public health access for over 66% of the population residing in rural areas. Given the opportunities for private investors to fill up the gaps in the sector, the private hospitals have grown in the last two decades, concentrated in the major Tier 1 and Tier 2 cities, observed to grow into 250 hospitals in 2020 from one to two private hospitals in the 1980s, according to report made by Okkar Thiri Co., Ltd on Covid-19 response.
Most of the public hospitals are not equipped with modern healthcare devices and equipment due to financial constraints and are dealing with shortage of doctors and nurses. The need for improved healthcare services is not just limited to hospitals and clinics, but also contains diagnostic centers and laboratories.
Challenges are on the way despite widespread public hospitals across the country and booming private healthcare services in cities with relatively higher earning capacity in remote areas. Most of the public hospitals are not equipped with modern healthcare devices and equipment due to financial constraints and are dealing with shortage of doctors and nurses. The need for improved healthcare services is not just limited to hospitals and clinics, but also contains diagnostic centers and laboratories. The capacity and ability of the National Health Laboratory that can provide quality diagnostic service and disease surveillance was limited. The country still counts on support from laboratories abroad. There are only two public laboratories, each in Yangon, and Mandalay. The National Health Laboratory saw further improvements last year when French Development Agency (AFD) and European Union (EU) granted concessional loans to MoHS to construct and rehabilitate the buildings of the NHL in Yangon and Mandalay. The new laboratories in Yangon, as well as the rehabilitated ones in Yangon and Mandalay, are expected to be fully operational in 2024.
There is a handful of hospitals providing radiation therapy in the country which includes Yangon General Hospital, Mandalay General Hospital (Mandalay), Sao San Htun Hospital (Taungyi), Nay Pyi Taw Hospital, and Pin Lon Hospital which is one of the private hospitals in Yangon. Yangon General Hospital is a major public hospital, with a few number of advanced imaging devices installed such as CT and MRT machines. MRI imaging has a role in the diagnosis, staging and follow-up of other tumors and more than 25,000 scanners are estimated to be in use worldwide. At public hospitals, diagnostic imaging tests such as X-ray & ultrasound are free for in-patients.
Effective, safe, and high quality imaging is important for much medical decision-making and can reduce unnecessary procedures. For example, some surgical interventions can be avoided altogether if simple diagnostic imaging services such as ultrasound are available. Per Myanmar’s Diagnostic Imaging & In-vitro Diagnostic (IVD) report recommendation, there is an increased penetration of IVD in Myanmar due to growing aging population and high prevalence of major diseases like diabetes, hypertension and cervical cancer. Top five causes of death per 100,000 population in 2017 for Myanmar are reportedly known as COPD, Stroke, Ischemic heart disease, Diabetes and Cirrhosis. The report continues that the upper middle class (representing ~10% of the population) get their IVD tests for specific diseases in Thailand and Singapore.
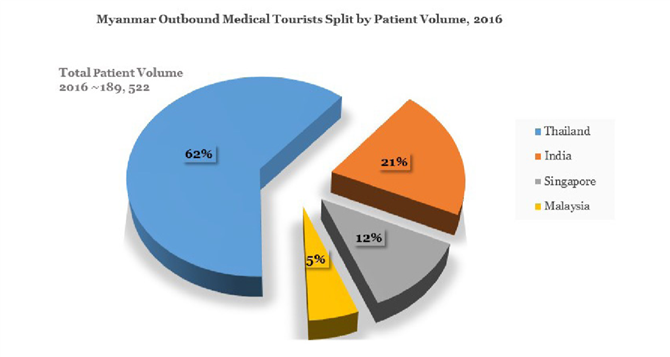
Outbound medical tourism is increasing in tandem with an influx of famous foreign hospitals in the medical providers sector as shown in figure. According to the Nation Thailand news report, “patients from Myanmar have so far spent an estimated $600 million on medical care abroad with expenditures accelerating,” Local medical experts commented the steady increase in seeking treatments abroad is due to trust issues in healthcare delivery.
Local news media reported people were gaining confidence in public health facilities in recent years. There were over 19 million people sought treatment at the country’s public hospitals and over 10,000 health centers in 2019, 9 million more than in 2016 according to Tun Maung Nyut, head of the Public Health Department in Shan State. Private hospitals account for 14% of total hospitals and contribute to 7% of total beds in Myanmar. Public hospitals account for ~86% of hospitals but are far behind regional quality standards.
So far, the pharmaceutical industry is in its infancy stage with significant underproduction of local pharmacies facing underdevelopment of supply chain and storage. Myanmar informally relies on imported medicines from neighbouring countries. It is one of the gray areas in the country where illicit trades of drugs are found. Traditional medicine of Myanmar also has an important agenda as regards service delivery as many rural people still rely on traditional herbal medicines.
Sailing into the Pandemic
The pandemic markedly strained the capacity at state-run hospitals as evident in the number of ICUs which is relatively small for Myanmar’s total population. “The rising demand for nurses in the healthcare sector has been important due to COVID-19 pandemic,” said in a statement by San San Yi, chairperson of Myanmar medical equipment distributor Okkar Thiri, to OBG. According to one of Myanmar Insider’s analysis articles, wearing facemasks is more beneficial and affordable means to contain the spreading as a non-pharmaceutical intervention in both developed nations and developing nations, be it fabrication of home-made, three-layered masks or surgical masks. The possibility of resurgence of second wave Covid-19 in the country is coming as there were new positive cases found in Sittwe region in Rakhine State, as of writing.










